Standardisation

The current diversity in vision testing methods and notations amongst eye care practitioners emphasizes the need for all professionals to adopt standardized vision tests and notations, according to international protocols.
Optonet is a collaborative project designed to encourage all healthcare practitioners involved in vision care to implement standardized vision tests and notations in their daily practice, in order to improve accuracy of measurements, as well as communication amongst professionals.
The Project is initially addressing visual acuity (VA) measurement, but is expected to expand to all main clinical procedures employed in the evaluation of the visual function for a general population.
Standarization in healthcare is acknowledged as one of the most effective methods of improving quality patient care while reducing costs. However, it may just be interesting to review how standardization may affect the most basic of the vision functions measured: Visual Acuity (VA).
The Importance of VA Standardization
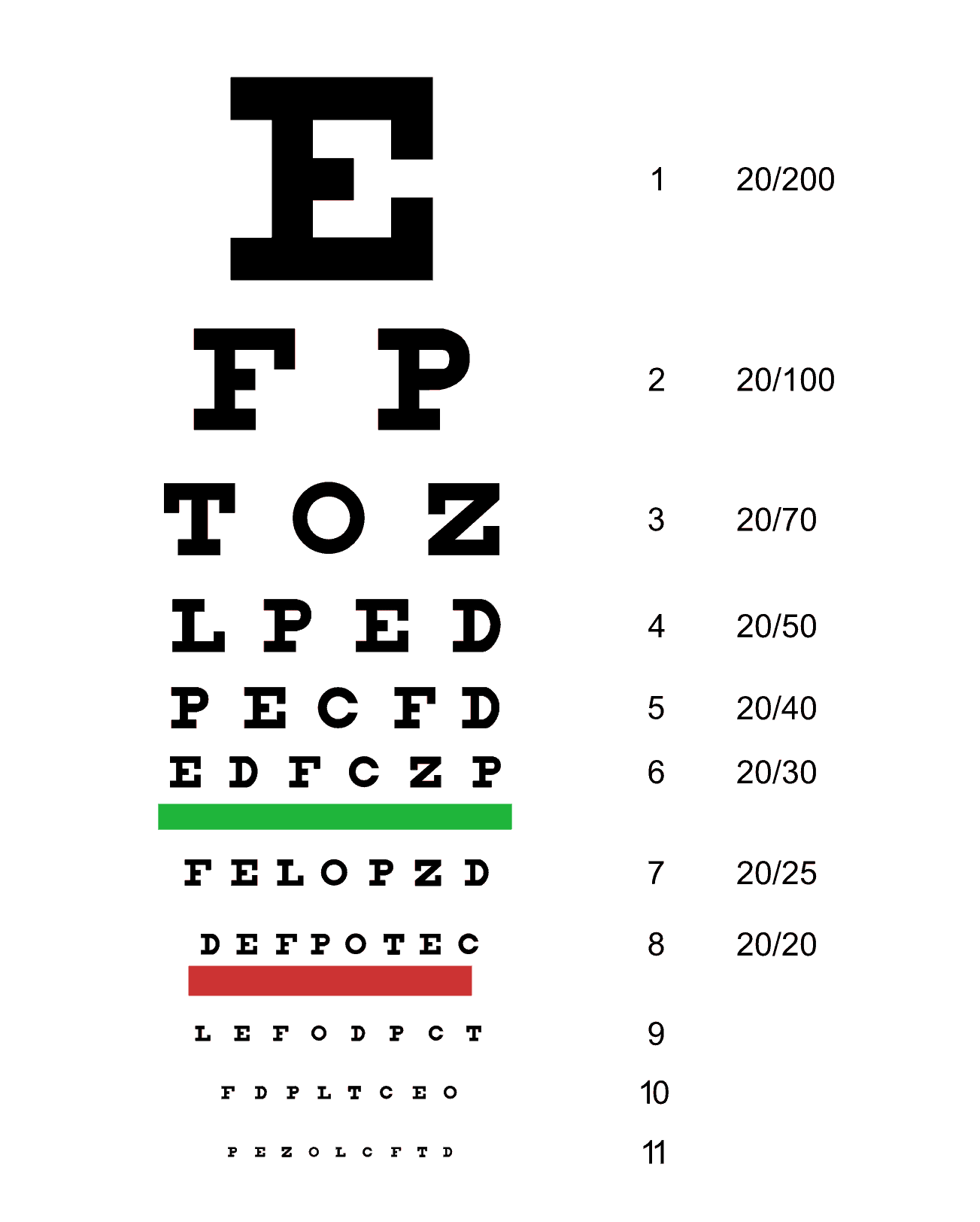
Visual Acuity (VA) is probably the single most important and useful measure of visual function and to that end is routinely used by health related professionals, both in clinical and research settings.
Unaided VA gives an estimate of the type and quantity of refractive error, whereas aided VA is used as a reference when searching for the optimum refractive correction in optometric testing. Corrected VA scores in relation to age1,2 provide information about the integrity of the ocular media and visual pathways, and help detect vision-threatening eye conditions.3 VA is also an indicator of quality of life: when it is reduced it gives a measure of the level of disability during daily live activities.4,5
Visual acuity measurements have huge economic and social implications: it is used for the diagnosis, prognosis and monitoring of eye disorders, the prescription of drugs, to assess the indication and outcome of ocular surgery (such as cataract or refractive surgery), and for the evaluation of ocular treatments, which range from occlusion therapy in amblyopia to high-cost pharmacological therapies.6 VA is even used to decide whether a person can drive a car or pilot a plane.
In regards to children, VA is included in virtually all public health screening programs, with the aim to detect amblyopia and/or significant refractive errors,7,8 and its value is indeed used as a criterion for referral for further evaluation and early treatment.9,10
Many important decisions are based on the measurement of visual acuity, and yet, up until now, the tests and scoring systems used by different practitioners were neither standard nor accurate, and often not even equivalent. The need for widespread use of standardized VA tests that may provide reliable and precise VA measurements is crucial;11 not only for recording correct initial values in a given patient, but also for identifying a true change in VA12 when a patient obtains a different score in another occasion and/or when checked by a different practitioner. This will also prevent unnecessary false positive and negative referrals amongst healthcare practitioners.
Furthermore, communication amongst different professionals involved in vision care requires that we all use standardized measurements of VA. Only then, exchange of patient data (e.g. between Optometrists and Ophthalmologists, or between clinicians and researchers) can take place in an effective and accurate manner. This will ultimately reflect on better patient care.
References
1. Elliott, D. B., Yang, K. C. & Whitaker, D. Visual acuity changes throughout adulthood in normal, healthy eyes: seeing beyond 6/6. Optom. Vis. Sci. Off. Publ. Am. Acad. Optom. 72, 186–191 (1995).
2. Ohlsson, J. & Villarreal, G. Normal visual acuity in 17–18 year olds. Acta Ophthalmol. Scand. 83, 487–491 (2005).
3. Ariyasu, R. G. et al. Sensitivity, specificity, and predictive values of screening tests for eye conditions in a clinic-based population. Ophthalmology 103, 1751–1760 (1996).
4. Hochberg, C. et al. Association of vision loss in glaucoma and age-related macular degeneration with IADL disability. Invest. Ophthalmol. Vis. Sci. 53, 3201–3206 (2012).
5. West, S. K. et al. Function and visual impairment in a population-based study of older adults. The SEE project. Salisbury Eye Evaluation. Invest. Ophthalmol. Vis. Sci. 38, 72–82 (1997).
6. Patel, P. J., Chen, F. K., Rubin, G. S. & Tufail, A. Intersession repeatability of visual acuity scores in age-related macular degeneration. Invest. Ophthalmol. Vis. Sci. 49, 4347–52 (2008).
7. Sonksen, P. M., Wade, A. M., Proffitt, R., Heavens, S. & Salt, A. T. The Sonksen logMAR test of visual acuity: II. Age norms from 2 years 9 months to 8 years. J. AAPOS Off. Publ. Am. Assoc. Pediatr. Ophthalmol. Strabismus Am. Assoc. Pediatr. Ophthalmol. Strabismus 12, 18–22 (2008).
8. Anstice, N. S. & Thompson, B. The measurement of visual acuity in children: an evidence-based update. Clin. Exp. Optom. J. Aust. Optom. Assoc. 97, 3–11 (2014).
9. Köhler, L. & Stigmar, G. Visual disorders in 7-year-old children with and without previous vision screening. Acta Paediatr. Scand. 67, 373–377 (1978).
10. Kvarnström, G., Jakobsson, P. & Lennerstrand, G. Visual screening of Swedish children: an ophthalmological evaluation. Acta Ophthalmol. Scand. 79, 240–244 (2001).
11. Ferris, F. L. & Bailey, I. Standardizing the measurement of visual acuity for clinical research studies: Guidelines from the Eye Care Technology Forum. Ophthalmology 103, 181–2 (1996).
12. Bailey, I. L., Bullimore, M. a, Raasch, T. W. & Taylor, H. R. Clinical grading and the effects of scaling. Invest. Ophthalmol. Vis. Sci. 32, 422–32 (1991).
Free Trial
Activate your Optonet Vision Unit today and discover its capabilities firsthand.
